Latest Features: Intraoral Scanning in Orthodontic Practice by Ricky E. Harrell, DMD, MA
An evidence-based evaluation of three-dimensional scanning technology in orthodontic practice.
An evidence-based evaluation of three-dimensional scanning technology in orthodontic practice.
One of the challenges in providing orthodontic treatment is deciding which technology to utilize. Considerations include the purchase and support of the technology, training, the chairtime and lab time required, and patient acceptance. With capital equipment, clinicians must ask if the technology is viable over an extended period, and if the return on investment is worth the expenditure. Intraoral scanning for three-dimensional (3D) orthodontic models is no different, as providers must weigh the commitment of time and resources needed to ensure its successful incorporation into orthodontic practice.
In 1984, computer aided design/computer aided manufacturing (CAD/CAM) entered the dental world with the advent of Chairside Economical Restoration of Esthetic Ceramics (or CEREC) restorations.1 The use of CAD/CAM technology primarily remained in the domain of restorative dentistry and did not make much impact on orthodontics until the 21st century. In 2001, technology was introduced to orthodontic practitioners that allowed the production of 3D digital models, indirect bonding trays and virtual occlusal setups. With this early 3D scanning capability, either stone models or polyvinyl siloxane (PVS) impressions were sent to the scanning center, where the model or impression was scanned. The data was processed into a digital file that was downloaded into the practitioner’s office network. The first in-office digital impression system capable of full-arch intraoral scanning came online in 2008.2 Technology subsequently evolved such that, by 2011, clinicians could submit 3D scans in lieu of PVS impressions for fabrication of aligners. Not long after this milestone, additional companies began offering programs for fabrication of fixed orthodontic appliances.
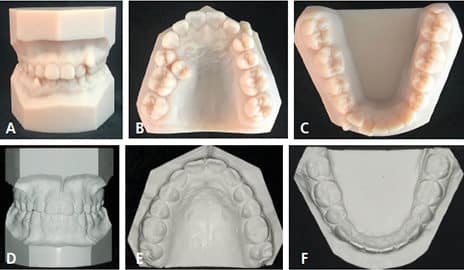
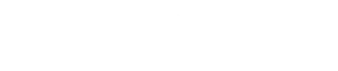
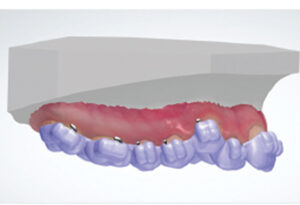
In today’s orthodontic practice, 3D intraoral scans are used for fabrication of orthodontic study models (Figures 1A through 1F), customized archwires, and customized fixed appliances (in both labial and lingual versions), as well as indirect bonding trays (Figure 2). In addition, digital technology is also used for diagnostic setups, fabricating aligners and removable orthodontic appliances, and diagnostic procedures (Figure 3, Figure 4 and Figure 5) in both orthodontic and orthodontic/orthognathic surgical combined treatment.
INTRAORAL SCANNING OVERVIEW
One of the initial drawbacks of 3D intraoral scanning was the need to apply a titanium dioxide powder to the dentition prior to scanning to ensure that light from the scanner was reflected back to the scanner wand in a uniform and predictable manner.3 The powder was considered objectionable by some patients, who saw similarities to having traditional impression material in their mouths.4 As long as the structures to be scanned are relatively clean and dry, many of the current intraoral scanners no longer require the application of powder.
Here is a brief description of dental scanning technologies:
Triangulation: Optical triangulation measures distances to objects without physically touching them. It is useful in acquiring data within a few microns from delicate, wet or soft materials, as are found in the oral cavity. Laser technology is used to calculate distances from the scanner wand sensor to the object using Pythagorean geometric principles.5,6
Active Wavefront Sampling: This system utilizes a 3D-in-motion technique. It captures the 3D data in a video sequence and models the data in real time. Because it does not rely on a laser and triangulation techniques, it is thus faster and eliminates the downsides of distortion and optical illusion. It can create an onscreen virtual model almost instantaneously.7
Parallel Confocal Imaging: Using a system of “point and stitch” reconstruction, laser light bounced off the target surface is reflected back to the sensor. The resulting data is used to construct thousands of tomographic slices that are assembled into a picture of the target object.8
Accordion Fringe Interferometry: This system utilizes two beams of laser light that create three projected patterns — called fringe patterns — that strike the target surface and take on new fringe patterns. The distortion in the original pattern is detected by a high-definition video camera, which forms the 3D image.9

All of the current dental scanners offer acceptable accuracy for prosthodontic and orthodontic utilization. Most will record their data in stereolithography (STL) files that are accepted by most laboratories.
SCANNING IN ORTHODONTICS
Prior to adaptation of any technology, practitioners must consider whether it offers advantages over existing methods. One benchmark is patient acceptance, and, specific to orthodontics, acceptance and tolerance of the technology in younger patients. In a study by Burhardt et al,4 38 subjects between the ages of 10 and 17 had both conventional alginate impressions and intraoral scans for diagnostic orthodontic models. The study showed that 29% of the subjects preferred the alginate impressions, 51% preferred intraoral scans, and 20% stated no preference. Reasons for preferring the intraoral scanner to conventional impressions included gag reflex, queasiness, difficulty breathing, uncomfortable breathing and anxiety with the conventional technique. Negative reactions to scanning were based on perception of scanning times.4 Similarly, a study by Farah and Brown10 showed that 75% of subjects comparing conventional impressions and intraoral scanning preferred scanning.
That noted, a different conclusion was reached by Grunheid et al.11 In a 2014 study evaluating accuracy, time and patient acceptance, the authors found that 73% of a group of 15 subjects ranging in age from 12 to 52 preferred traditional impressions to intraoral scanning. When relating issues of discomfort, 33% of the traditional impression group reported being “somewhat uncomfortable;” this compares to 40% of the scanner group that described the procedure as “somewhat uncomfortable.” It should be noted, however, that all of the intraoral scans used to determine these results required the use of an intraoral powder technique — which may have affected patient perception.
In orthodontic practice, clinicians must also take into consideration the attitudes and perceptions of the dental auxiliaries who will be taking the bulk of impressions for diagnostic models. Although little research exists regarding assistants’ preference for traditional impressions or digital scanning, there is research on the attitude of dental students and faculty on this subject. Do students, many of whom fall into the millennial category, have a preference for intraoral scanning versus conventional impressions for crown and bridge working models? A study by Lee et al12 of dental students and clinicians showed that both groups felt that digital impressions involved the same degree of difficulty as conventional techniques. However, 77% of the students stated they were more effective with digital scanning than using conventional impression techniques for implant models. It should be noted that although similar in technique, the scan for an implant — which was the subject in this study — is different than a scan for a full-arch impression.

Another consideration before adopting a new technique or technology is whether the end results are as accurate, or more accurate, with the new technique. This issue has been resolved in a number of studies in the orthodontic realm, as well as prosthodontics and oral surgery. It is well documented that 3D-printed models from impressions are as accurate as plaster models generated from the same impressions.13 The accuracy of digital models made from intraoral scans is no longer in question, as they have been shown to be as accurate as plaster models made from traditional impression techniques — thus, such models are acceptable for orthodontic diagnostic purposes.14–17 As indicated by a systematic review of the literature, some authors have even suggested that digital models from intraoral scans are the new gold standard in orthodontics due to their accuracy and other perceived benefits — such as cost, time and storage considerations.18 This is because storage of conventional models can prove challenging. On average, model boxes require 95 to 115 cubic inches of space (Figure 6). In a large orthodontic practice, where thousands of patients will be treated within a relatively short period, model storage becomes unwieldy and problematic. Digital models shift the burden to virtual storage.
TREATMENT PLANNING
Another major consideration when adopting new technology is whether it will impact treatment-planning decisions. Providers must consider possible bias that might be influenced by use of handheld plaster models, handheld 3D-printed models or virtual 3D models. At present, it is unclear if this is a significant factor. A systematic review of decision-making found that treatment planning for orthognathic/orthodontic care changed in 13% to 22% of cases based on whether records were presented in a digital or plaster format. In orthodontic-only care, treatment planning changed in 6% of the cases reviewed, depending on the dental model type used (digital versus plaster).19

There are certainly other considerations when deciding between a digital and traditional impression format. A cost analysis should include the initial purchase of a scanner, software licensing, personnel time and training, data storage, and maintenance of the equipment. Costs for today’s intraoral scanners range from approximately $16,500 to $49,000. Licensing fees also have to be taken into account. Some firms provide free service initially, some charge per click, and others have a set monthly fee for software ranging from $1200 per year for the first two years to $3600 per year after two years.
A key advantage of digital technology is that it eliminates or minimizes the need to send impressions or poured models to the laboratory via mail or courier. Once the STL file is uploaded, it can be transferred to the lab with a click for model or appliance fabrication. Replacement of a retainer is an easy task (provided there has not been significant tooth movement), as the digital file is stored either locally, in the cloud, or at the lab for simple retrieval.
Two factors have made digital scanning an easy choice for large orthodontic practices. One deals with possible contamination, and the other involves costs. The use of physical models raises questions about asepsis, both in the clinic with trays, mixing bowls and wrapping, as well as the laboratory. Clinicians may experience uncertainty over potential contamination of model trimmers or appliances, or the possibility of models being made from nondisinfected impressions if there is a breakdown in the disinfection/sterilization cycle (Figure 7).
Another issue facing large practices is the question of how much lab expense and/or personnel time and effort should be directed toward the fabrication of models. Now that there is no longer going to be a required presentation of treated cases for the American Board of Orthodontics Examination Part III Clinical Exam, the pressure for clinicians to produce beautiful, highly polished orthodontic models is diminished.20 Prior to the change in the examination process, digitally produced models had become acceptable for submission — provided they met certain requirements in regard to detail, color, composition and basing.
DRAWBACKS OF INTRAORAL SCANNING AND DIGITAL MODELS

As was pointed out by Grunheid et al,11 3D scanning is neither universally welcomed by patients, nor does it always present significant savings in time or expenses. If physical models are required (for whatever reason) as opposed to virtual models, the cost from the laboratory is about the same for presentation-quality models. Depending on the number of scans required for any given clinic period, there can be significant delays in patient chairtime while waiting for a scanner to become available and undergo asepsis procedures between patients. It is much easier to have an adequate number of impression trays and impression materials than it is to have a significant number of scanners.
With the use of 3D scanning for diagnostic models and progress models (especially for patients undergoing orthognathic surgery), there is difficulty in reconciliation of the bite from centric occlusion to centric relation. Models mounted in centric relation on semi-adjustable or fully adjustable articulators using a centric relation bite and facebow transfer have long been the workhorse of orthodontists with patients for whom centric relation and centric occlusion are not coincident. With virtual models, the ability to fabricate splints in-office for diagnostic or treatment modalities is lost without 3D-printing capabilities. In this case, STL files must be sent out for fabrication of the prostheses, without plaster model and articulators in the laboratory. Often, intermediate splints for orthognathic surgery are constructed at a site distant from the oral surgeon. A different system of planning for these limitations of 3D imaging has to be in place in order for the clinical team to function in a timely fashion.
It has been demonstrated that tooth excursions replicated on a virtual articulator are similar and as accurate as those done on a physical articulator. Delong et al21 noted that occlusal contacts derived from stone models on an articulator were faithfully reproduced on virtually mounted 3D models. The same conclusion was reached by Maestre-Ferrin et al22 in a study that suggested, “The virtual articulator is a precise tool for the full analysis of occlusion in a real patient.” These same findings with regard to accuracy of articulated virtual versus stone models for orthognathic surgery planning have been verified by Caloss et al,23 as well as the previously mentioned study by Delong et al.21
From a clinician’s perspective, unless in-office fabrication is available or a lab facility is on site that can print models, turnaround time for appliances must be considered in treatment planning. While 3D-printed appliances are as accurate as handcrafted appliances, often, they cannot be produced as quickly when employing a local laboratory.24,25 In such cases, scheduling for appliance delivery becomes difficult when it is not planned well in advance.
SUMMARY
Once chiefly thought of in terms of restorative procedures, intraoral scanning has become an integral part of orthodontics. In today’s practice, 3D intraoral scans are used for fabrication of fixed appliances and orthodontic study models, as well as indirect bonding trays. This technology is also useful in diagnostic setups, fabrication of aligners and removable orthodontic appliances, and diagnostic procedures. While clinicians should be well versed in traditional impression techniques, the need for digital skills is likely to assume an increasingly important role in evidence-based orthodontic care.
KEY TAKEAWAYS
- Intraoral scans can be used for fabrication of orthodontic study models, aligners and other appliances, as well as indirect bonding trays.
- The accuracy of digital models made from intraoral scans has been shown to be as accurate as plaster models made with traditional impression techniques; thus, digital
models are acceptable for orthodontic diagnostic procedures.14–17 - A key advantage of digital technology is that it eliminates or minimizes the need to send impressions or poured models to the laboratory via mail or courier. Once
the digital file is uploaded, it can be transferred to the lab with a click for model or appliance fabrication. - While clinicians should be well versed in traditional impression techniques, the need for digital skills is likely to assume an increasingly important role in orthodontic treatment.
REFERENCES
- Mörmann W, Brandestini M, Ferru A, Lutz F, Krejci I. Marginal adaptation of adhesive porcelain inlays in vitro. Schweiz Monatsschr Zahnmed. 1985;95:1118–1129.
- Jones P. The iTero optical scanner for use with Invisalign: a descriptive review. Dental Implantol Update. 2008;19:1–4.
- Powder for enhancing feature contrast for intraoral digital image scanning. U.S. Patent Application #US13433643: 2012-03-29. Available at: https://patents.google.com/patent/WO2013148150A1/en. Accessed June 7, 2018.
- Burhardt L, Livas C, Kerdijk W, van der Meer WJ, Ren Y. Treatment comfort, time perception, and preference for conventional and digital impression techniques: a comparative study in young patients. Am J Orthod Dentofac Orthop. 2016;150:261–267.
- Taneva E, Kusnoto B, Evans CA. 3D Scanning, imaging, and printing in orthodontics. Issues in contemporary orthodontics. Available at: intechopen.com/books/issues-in-contemporary-orthodontics/3d-scanning-imaging-and-printing-in-orthodontics. Accessed June 7, 2018.
- Kravitz ND, Groth C, Jones PE, Graham JW, Redmond WR. Intraoral digital scanners. J Clin Orthod. 2014;48:337–347.
- Birnbaum NS, Aaronson HB. Dental impressions using 3D digital scanners: virtual becomes reality. Compend Contin Educ Dent. 2008;29: 484–505.
- Ting-Shu S, Jian S. Intraoral digital impression technique: a review. J Prosthodont. 2015;24:313–321.
- Logozzo S, Franceschini G, Kilpelä A, Caponi M, Governi L, Blois L. A comparative analysis of intraoral 3D digital scanners for restorative dentistry. Internet J Med Tech. 2008;5:1–18.
- Farah J, Brown L. Integrating the 3M ESPE chairside oral scanner C.O.S. into daily clinical practice. Dent Advisor. 2009;12:1–4.
- Grunheid T, McCatrthy S, Larson BE. Clinical use of a direct chairside oral scanner: an assessment of accuracy, time, and patient acceptance. Am J Orthod Dentofac Orthop. 2014;146:673–682.
- Lee SJ, MacArthur RX, Gallucci GO. An evaluation of student and clinical perception of digital and conventional implant impressions. J Prosthet Dent. 2013;110:420–423.
- Dalstra M, Melsen B. From alginate impressions to digital virtual models: accuracy and reproducibility. J Orthod. 2009;36:36–41.
- Zilberman O, Huggare JAV, Parikakis KA. Evluation of the validity of tooth size and arch width measurements using conventional and three-dimensional virtual orthodontic models. Angle Orthod. 2003;73:301–306.
- Fleming PS, Marinho V, Johal A. Orthodontic measurements on digital study models compared with plaster models: a systematic review. Orthod Craniofac Res. 2011;14:1–16.
- Ender A, Mehl A. In-vitro evaluation of the accuracy of conventional and digital methods of obtaining full-arch dental impressions. Quintessence Int. 2015;46:9–17.
- Cuperus AM, Harms MC, Rangel FA, Bronkhorst EM, Schols JG, Breuning KH. Dental models made with an intraoral scanner: a validation study. Am J Orthod Dentofacial Orthop. 2012;142:308–313.
- Rossini G, Parrini S, Castroflorio T, Deregivus A, Debermardi CL. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: a systematic review. Am J Orthod Dentofacial Orthop. 2016;149:161–170.
- Pachêco-Pereira C, De Luca Canto G, Major PW, Flores-Mir C. Variation of orthodontic treatment decision-making based on dental model type: a systematic review. Angle Orthod. 2015;85:501–509.
- Chung CH, Tadlock LP, Barone N, et al. American Board of Orthodontics: time for change. Am J Orthod Dentofacial Orthop. 2018;153:321–323.
- Delong R, Ko CC, Hodges JS, Douglas WH. Comparing maximum intercuspal contacts of virtual dental patients and mounted dental casts. J Prosthet Dent. 2002;88:622–630.
- Maestre-Ferrin L, Romero-Millán J, Peñarrocha-Oltra D, Peñarrocha-Diago M. Virtual articulator for the analysis of dental occlusion: an update. Med Oral Patol Oral Cir Bucal. 2012;17:e160–e163.
- Caloss R, Duan Y, Parthasarthy J, Jing WS. Comparison of 3D computer-assisted virtual planning and articulated model planning for bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 2014;72:e44–e45.
- Nasef AA, El-Beialy AR, Mostafa YA. Virtual techniques for designing and fabricating a retainer. Am J Orthod Dentofacial Orthop. 2014;146:394–348.
- Lauren M, McIntyre F. A new computer-assisted method for design and fabrication of occlusal splints. Am J Orthod Dentofacial Orthop. 2008;133 (Suppl 4):S130–S135.
The author has no commercial conflicts of interest to disclose.
Featured Image by YAKUBOVALIM/ISTOCK/GETTY IMAGES PLUS
Decisions in Dentistry, September 2018
Click Here for Original article
GSO Experts

Dr. Ricky E. Harrell//
Program Director Emeritus,
Diplomate of the ABO