Temporary anchorage devices (TADs) are generally miniscrews placed in either alveolar or extra-alveolar bone for the purpose of providing orthodontic anchorage. The hallmark of this device is its intended removal once it has completed its function in the treatment regimen. This is opposed to a dental implant that serves as an anchor device with the intention of utilization as a dental prosthesis following its use as an orthodontic anchor. This article will focus on TAD design, placement and some of the ways in which these devices are currently used in orthodontic procedures.
Although TADs have been in existence for more than 35 years, it is only within the past decade that their use has become commonplace among orthodontic practitioners in the United States. In a 2008 survey of members of the American Association of Orthodontists, Buschang et al1 determined that 80% of respondents had at least one miniscrew case in their practice. More than half of those surveyed (564 members responded) had placed 10 or fewer TADs themselves. The majority of orthodontists who responded positively to using TADs had referred the placement to either an oral surgeon (49.4%) or periodontist (15.8%), with about 35% personally placing the first miniscrew in their practice.
In a later paper by Shirck et al2 in 2011, surveys concerning TADs usage were sent to the 61 accredited orthodontic residency programs in the U.S., and to 61 orthodontic practitioners. Based on a response rate of 70.4% for the orthodontic residencies and 63.9% for the private practitioners, the usage rate of TADs in orthodontic treatment was 82.9% for the residencies and 69.2% for private practitioners. Usage rate in the patient population under treatment was 5.3% of patients being treated in the residency programs and 6% of patients being treated in private practice.
In the 2008 survey, the main reason for nonutilization of TADs by orthodontists was a reported lack of training within residency programs.1 These programs began to see the impact of TADs on orthodontic practice and, by 2011, more than 80% had incorporated formal training in their didactic/research curriculum — which would suggest future practitioners will be well versed in the use of TADS in orthodontic treatment.2
WHY USE THESE DEVICES?
Orthodontic tooth movement is grounded in the laws of biology and physics. Newton’s Third Law of Motion states that “all forces between two objects exist in equal magnitude and opposite direction” — in other words, “for every action, there is an equal and opposite reaction.” In orthodontic treatment, the goal is for a certain tooth or group of teeth to move in the desired direction. To affect this movement, some force has to be applied to both the tooth or teeth to be moved (the “active” unit) and either a tooth, group of teeth or extraoral force (such as headgear or a facemask) to resist that movement (the “reactive” unit). The ability of the reactive unit to resist movement is termed anchorage. In practice, the undesired movement of the reactive unit has plagued orthodontists since the creation of the specialty, because such movement often leads to undesirable changes in the proposed occlusal scheme.3
In 1923, Ottofy4 defined anchorage as “the base against which orthodontic force or reaction of orthodontic force is applied.” Daskalogiannakis5 defined anchorage as “resistance to unwanted tooth movement.” One of the problems in traditional orthodontic treatment without TADs is the difficulty in effecting tooth movement in only one direction. An example would be retraction of a maxillary canine into the extraction space of the adjacent first bicuspid without the teeth posterior to the extraction space moving anteriorly. In maxillary first bicuspid extraction treatment, it is estimated that as much as 35% of the space is lost to mesial movement of the teeth posterior to the extraction space — even with maximum anchorage considerations utilized. Extraction space closure due to anchorage loss has been estimated at one-third of the space for first bicuspid extraction and one-half for second bicuspid extractions, even with efforts made to preserve anchorage.6
One of the ways to minimize anchorage loss is the use of auxiliary appliances to the posterior anchor unit, including headgear or fixed auxiliaries, such as a transpalatal arch or Nance button.7 The use of multiple teeth at the anchorage segment to form a large counterbalancing unit and the application of differential moments have also been described as methods to stabilize molar position.8–10 However, even with excellent cooperation, space loss due to anchor units moving is almost inevitable. The use of TADs provides a solution to much of the anchor loss situation, as well as allowing tooth movement previously not possible.11–14
Although skeletal anchorage plates are grouped with TADs (as they are also removed after their objectives are accomplished), their review is beyond the scope of this paper.
DEVICE DESIGN
Miniscrews or TADs are generally made of titanium or titanium alloy to ensure they are bioinert (i.e., they will not elicit an inflammatory tissue response or discharge corrosive by-products into the bone or surrounding tissue).15 Ranging from 4 to 20 mm in length (6 to 12 mm being the most common) and 1.0 to 2.3 mm in width, TADs will have a male-type head that fits into a female socket on a handheld driver for insertion (Figure 1). Almost all miniscrews commercially available are both self-drilling (no pilot hole necessary) and self-tapping (meaning, they produce the space for their threads by compression or cutting as they are inserted).16

Two thread types are utilized in TADs. The first is a cutting-type thread outline that is used on screws of larger diameter and length for placement into dense cortical bone. These threads will cut and remove small amounts of bone as the screw is inserted. The second type has a thread-forming outline which compresses less-dense bone as it is inserted through a smaller amount of cortical bone during TAD placement.
LOCATION AND INSERTION
These devices may be inserted into alveolar bone and extra-alveolar bone in the maxilla or mandible. In the mandible, the majority are placed into inter-radicular bone, with the cortical bone increasing in thickness as it moves from the midline posteriorly. The thickest cortical bone, as determined by cone beam computed tomography studies, is located approximately 6 mm apical to the alveolar bone crest.17 Other areas in the mandible utilized for placement of TADs include (but are not limited to) the mandibular symphysis, anterior external oblique ridge and retromolar area of the alveolar crest.18
In the maxilla, alveolar bone is generally adequate for placement, with bone levels thinnest in the maxillary anterior region and increasing in thickness toward the posterior of the arch. However, bone thins in the maxillary posterior alveolus at 4 mm from the alveolar bone crest, as opposed to bone measured from the alveolar crest at 2 mm and 6 mm apically. One extra-alveolar site that has gained popularity among clinicians due to increased bone thickness is the palate, with the thickest bone located antero-posteriorly at the region of the maxillary bicuspids and parasagitally from 2 to 8 mm from the midline of the palate.19 Other extra-alveolar sites in the maxilla include the infrazygomatic ridge, incisive fossa and canine fossa.18
As noted, the majority of TADs on the market do not require a pilot hole unless placing a large-diameter (e.g., 2 mm) device into dense bone. Although TADs may be placed into the attached gingiva (preferred, if possible) or mucosa, if the mucosa is mobile, the TAD will often eventually be covered by soft tissue, making alteration of orthodontic treatment mechanics difficult without surgically uncovering the screw head.20 A transmucosal bar has been developed by Costa, Pasta and Bergamaschi to address this issue.21
There is controversy among practitioners who place TADs as to which angle of insertion provides the greatest stability. Some operators and researchers believe that all TADs should be inserted perpendicular to the cortical plate.22–24 Others feel that a more oblique angle of insertion is preferable, as it slightly increases thread contact with the cortical bone.25 This contact — defined as primary stability — is chiefly responsible for stability of the miniscrew, as they are not designed to osseointegrate.26 Regardless of the insertion angle, the surrounding bone must be healthy and uncompromised to withstand the force generated through the screws.
The use of anesthesia in TAD procedures is also controversial. Some practitioners believe that 20% benzocaine or compounded “super-topicals” provide adequate anesthesia for placement.27 Others assert that local anesthesia is more appropriate. Local agents can be administered via conventional needle injection or via a needleless device. The argument for using topicals only is the patient can feel if the screw contacts a root. However, the operator will also feel a change in resistance to insertion. Lamberton et al28 report that patients perceive less discomfort when local anesthesia is utilized for TADs placement in the buccal cortical plates. Anesthesia with topicals is also difficult on the palate, where areas of palatal mucosa can reach significant thickness.
The devices are inserted through the attached gingiva or mucosa, using a manual driver or, in some cases, a reduction handpiece. Recommended torque force, which can be measured with the handpiece, is in the range of 15 to 20 N/cm.29 The miniscrew is inserted up to the mucosal collar and checked for primary stability (i.e., tightness of the insertion). Most operators load the TAD immediately with an orthodontic force, although some applications require an impression and a model with an analogue for the TAD that is sent to a laboratory for fabrication of a TAD-supported appliance.
Although various articles report TAD success and failure data, success rates vary according to any number of factors — including bone health and thickness, mucosal insertion versus insertion through attached gingiva, immediate versus delayed loading and total loading. According to Antoszewska et al,30 success rates are reported to range between 75% and 94% in the literature.
CLINICAL APPLICATION
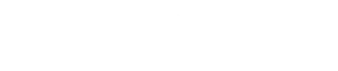
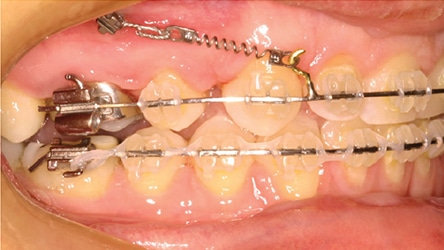
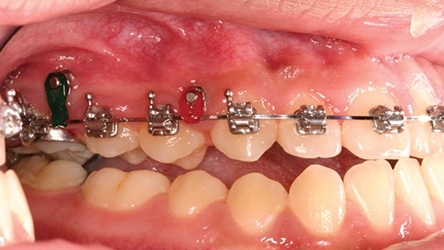
Anterior Retraction: According to the 2011 survey by Shirck et al,2 the most common use for TADs is anterior retraction in cases in which bicuspids have been extracted, or the occasional case with generalized spacing where anchorage concerns are significant. Retraction of the anterior teeth with TADs can be performed in two general ways. In the first, called indirect anchorage, the traditional teeth comprising the anchorage or reactive unit are tied to the TAD; that is, the unit to be moved is not attached directly to the TAD (Figure 2 and Figure 3). With this approach, traditional orthodontic biomechanics may be utilized without anchorage loss. The second approach is called direct anchorage. In this case, the active unit is attached to the TAD and bypasses anchorage to the other teeth. When using this method, clinicians must exercise great caution with regards to biomechanical principles (Figure 4 and Figure 5).
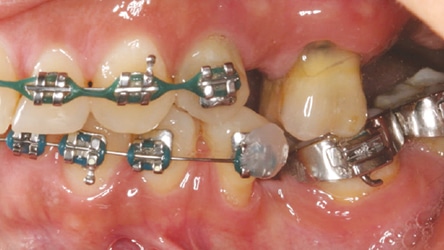
Protraction of Posterior Teeth: In this clinical situation, posterior teeth are moved anteriorly, often to prevent having to place an implant and a lifetime of maintenance for a young patient. One of the promising uses of TADs for protraction occurs when a primary second molar is lost and there is no second bicuspid to replace it. Whether or not teeth are missing in the opposing quadrant will dictate the eventual molar relationship. In the example shown, both the maxillary second bicuspid and mandibular second bicuspid are missing and a TAD was used for direct anchorage to protract the mandibular first and second molars (Figure 6 and Figure 7).
Molar or Posterior Arch Intrusion: In conjunction with prosthodontic replacement of teeth, it is often necessary to intrude hyper-erupted unopposed teeth in an opposing arch. Often, teeth can be restored to an appropriate occlusal plane without reduction in crown height or endodontic therapy prior to placing a bridge or implant in the opposing arch (Figure 8 and Figure 9). It is also a useful procedure in correcting occlusal cants (Figure 10 and Figure 11), as well as intrusion of posterior teeth for open-bite correction (Figure 12 and Figure 13).
Molar Distalization for Class II Correction: There are a number of ways to utilize TADs for molar distalization for a Class II dental correction. Currently popular is the use of a palatal TAD(s) attached to a transpalatal arch that is bonded to the second or first bicuspids. The palatal approach has become more popular due to the excellent bone stock found in the parasaggital area in the bicuspid region. Class II correction appliances, as well as fixed appliances, are compatible with TAD anchorage, as well.

Anterior Intrusion for Deep Bite Correction: These devices are very useful (using either a direct anchorage or an indirect anchorage) for intrusion of anterior teeth for correction of a deep overbite. This is particularly helpful in patients with excessive gingival display and maxillary incisor display with the lips in repose. Typically, TADs can be used with direct anchorage to the maxillary incisor segment, or an indirect anchorage can be utilized when an intrusion auxiliary arch is utilized for incisor intrusion.
ADDITIONAL USES
One of the most promising uses of TADs is with expansion appliance anchorage in patients who were once thought to be past the age at which the palate can be expanded. Sutural separation has been documented in these patients at a more advanced age than was once thought possible —again expanding the boundaries of traditional orthodontics.
This clinical approach is also useful for temporary implant purposes. One of the dilemmas facing orthodontists is how to maintain space during the retention period, when a patient has completed orthodontic treatment, but is too young for placement of an osseointegrated implant with a prosthesis for long-term restoration. Pontics can be fabricated to fit onto a TAD and utilized for several years while the patient continues growth and passive eruption of the teeth. Although there is some degree of diminishing vertical bone growth directly adjacent to the TAD (usually on the order of 1 mm), that area is removed when the implant is placed so there is minimal clinical disruption to the surrounding bone (Figure 14).

Other uses for TADs include uprighting molars, appliance anchorage, eruption of impacted teeth, assisting in tooth movement to shift maxillary and mandibular midlines, and as attachments for elastics in condylar fractures in young patients (especially those in whom all permanent dentition has erupted), essentially replacing archbars and their accompanying undesirable sequellae.
SUMMARY
The use of TADs can no longer be considered a fad in contemporary orthodontics. They have expanded the capabilities of clinicians who are familiar and comfortable with their use. They have allowed the correction of some borderline orthognathic surgery patients to be treated with an orthodontics-only approach. It took some time before their use became commonplace in orthodontics. As the younger generation of orthodontists enter practice and the academic arenas, TAD use will continue to increase if trends continue as they have in the past several years.
In summation, the use of TADs has made orthodontic anchorage less reliant upon patient cooperation. While they do not necessarily increase the rate of orthodontic correction, they allow clinicians to achieve better and more predictable outcomes. For these reasons, TADs will continue to be a part of the regimen of contemporary orthodontic practice.
KEY TAKEAWAYS
- Placed in either alveolar or extra-alveolar bone for the purpose of providing orthodontic anchorage, temporary anchorage devices (TADs) are removed once they complete their function in the treatment regimen.
- Generally made of titanium or titanium alloy, TADS are inserted through the attached gingiva or mucosa using a manual driver or, in some cases, a reduction handpiece.
- The most common use is for anterior retraction in cases in which bicuspids have been extracted, or the occasional case with generalized spacing where anchorage concerns are significant.2
- These devices are also useful for intrusion of anterior teeth for correction of a deep overbite.
- There is controversy among practitioners who place TADs as to which angle of insertion provides the greatest stability, and which anesthetic technique is best
- While they do not necessarily increase the rate of orthodontic correction, TADs allow tooth movement previously not possible11–14 and contribute to more predictable outcomes.
References
- Buschang PH, Carrillo R, Ozenbaugh B, Rossouw PE. 2008 Survey of AAO members on miniscrew usage. J Clin Orthod. 2008;42:513–518.
- Schirk JM, Firestone AR, Beck FM, Vig KW, Huja SS. Temporary anchorage device utilization: Comparison of usage in orthodontic programs and private practice. Orthodontics (Chic.). 2011;12:222–231.
- Cope JB. Temporary anchorage devices in orthodontics: A paradigm shift. Semin Orthod. 2005;11:3–9.
- Ottofy L. Standard Dental Dictionary. Chicago, IL: Laird and Lee Inc; 1923.
- Daskalogiannakis J. Glossary of Orthodontic Terms. Chicago, IL: Quintessence Publishing Co; 2000.
- Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod. 1997;31:586–608.
- Geron S, Shpack N, Samouil K, Davidovitch M, Vardimon AD. Anchorage loss — A multifactorial response. Angle Orthod. 2003;73:730–737.
- Nanda R, Kuhlberg A. Biomechanical basis of extraction closure. In: Nanda R, Kuhlberg A, eds. Biomechanics in Clinical Orthodontics. Philadelphia, PA: WB Saunders; 1996;156–187.
- Hart A, Taft L, Greenberg SN. The effectiveness of differential moments in establishing and maintaining anchorage. Am J Orthod Dentofacial Orthop. 1992;112:434–442.
- Rajcich MM, Sadowsky C. Efficacy of intraarch mechanics using differential moments for achieving anchorage control in extraction cases. Am J Orthod Dentofacial Orthop. 1997;112:441–448.
- Kanomi R. Mini–implant for orthodontic anchorage. J Clin Orthod. 1997;31:763–767.
- Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201–209.
- Kyung HM, Park HS, Bae SM, Sung JH, Kim IB. Development of orthodontic micro-implants for intraoral anchorage. J Clin Orthod. 2003;37:321–328.
- Carano A, Velo S, Incorvati C, Poggio P. Clinical applications of the Mini-Screw-Anchorage-System (MAS) in the maxillary alveolar bone. Prog Orthod. 2004;5:212–235.
- Silverstein J, Barreto O, Franca R. Miniscrews for orthodontic anchorage: nanoscale chemical surface analyses. Eu J Orthod. 2016;38:146–153.
- Whang CZ, Bister D, Sherriff M. An in vitro investigation of peak insertion torque values of six commercially available mini-implants. Eur J Orthod. 2010;33:660–666.
- Baumgaertal S, Hans MG. Buccal cortical bone thickness for mini-implant placement. Am J Orthod Dentofacial Orthop. 2009;136:230–235.
- Papadopoulos MA, Tarawneh F. The use of miniscrew implants for temporary skeletal anchorage in orthdontics: A comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e6–e15.
- Baumgaertel S. Cortical bone thickness and bone depth of the posterior palatal alveolar process for mini-implant placement in adults. Am J Orthod Dentofacial Orthop. 2011;140:806–811.
- Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130:18–25.
- Costa A, Pasta G, Bergamaschi. Intraoral hard and soft tissue depths for temporary anchorage devices. Semin Orthod. 2005;11:10–15.
- Petrey JS, Saunders MM, Kluemper GT, Cunningham LL, Beeman CS. Temporary anchorage device insertion variables: effects on retention. Angle Orthod. 2010;80:634–641.
- Lee J, Kim JK, Choi YJ, Kim KH, Chung CJ. Effects of placement angle and direction of orthopedic force application on the stability of orthodontic miniscrews. Angle Orthod. 2013;83:667–673.
- Noble J, Karaiskos NE, Hassard TH, Hechter FJ, Wiltshire WA. Stress on bone from placement and removal of orthodontic miniscrews at different angulations. J Clin Orthod. 2009;43:332–334.
- Deguchi T, Nasu M, Murakami K, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. Am J Orthod Dentofacial Orthop. 2006;129:e7–e12.
- Migliorate M, Signori A, Silvestrini-Biavati A. Temporary anchorage device stability: an evaluation of thread shape factor. Eur J Orthod. 2012;34:582–586.
- Reznik DS, Jeske AH, Chen JW, English J. Comparative efficacy of 2 topical anesthetics for the placement of orthodontic temporary anchorage devices. Anesth Prog. 2009;56:81–85.
- Lamberton JA, Oesterle LJ, Shellhart WC, et al. Comparison of pain perception during miniscrew placement in orthodontic patients with a visual analog scale survey between compound topical and needle-injected anesthetics: A crossover, prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2016;149:15–23.
- Anka G. Use of miniscrews as temporary anchorage devices in orthodontic practice: I–Introduction. Aust Orthod J. 2006;22:131–139.
- Antoszewska J, Papadopoulos MA, Park HS, Ludwig B. Five year experience with orthodontic miniscrew implants: A retrospective investigation of factors influencing success rates. Am J Orthod Dentofacial Orthop. 2009;136:158e1–158e10.
The author has no commercial conflicts of interest to disclose.
FEATURED IMAGE BY HDESERT/ISTOCK/GETTY IMAGES PLUS
From Decisions in Dentistry. May 2017;3(5):15–16,18, 21–23.
Click Here for original article